November is Lung Cancer Awareness Month. We have learned a lot about how to prevent lung cancer-don’t smoke, and if you do smoke, quit. However, the disease is often not diagnosed until it is advanced or has spread to other parts of the body. Screening for lung cancer can help us to identify cases earlier in those at the highest risk for developing the disease. This can improve overall outcomes and quality of life.
In recent years, insurance companies have started to cover the cost of annual screening for certain people known to be at a higher risk for developing lung cancer. The guidelines as to who is “higher risk” and thus eligible for free preventive screening varies by types of insurance.
- For Employer Sponsored Plans, Individual Plans, and Marketplace (Obamacare) Plans
- Must be between the ages of 55-80
- Must have a 30 pack year history of smoking (1 pack per day for 30 years; 2 packs per day for 15 years, etc.)
- Are a current smoker, or have quit within the last 15 years
- For Medicare
- Must be between the ages of 65-77
- Must have a 30 pack year history of smoking (1 pack per day for 30 years; 2 packs per day for 15 years, etc.)
- Are a current smoker, or have quit within the last 15 years
- Have no signs or symptoms of lung cancer
- For Medicare Advantage plans
- These plans are not required to cover screening for those over the age of 70. It is best to check with your plan directly about their screening guidelines.
- Medicare Advantage plans may also charge copays, coinsurance or deductibles if you go out of network for your screening test Be sure to check which providers are in network before going for any procedure.
- For Medicaid
- Coverage for lung cancer screening varies from state to state. To find out if screening if covered, contact your state Medicaid program. There may be fees associated with these tests.
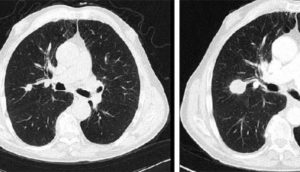
According to the CDC, “the only recommended screening test for lung cancer is low-dose computed tomography (also called a low-dose CT scan, or LDCT). In this test, an X-ray machine scans the body and uses low doses of radiation to make detailed pictures of the lungs.”
The risks involved with screening are small, but include a false positive diagnosis (test says there is cancer, but there isn’t), over diagnosis (meaning the test reveals an abnormality that would not cause the patient significant health problems) and exposure to radiation. The guidelines for screening are designed to offer the test to people most likely to benefit from screening. The CDC also recommends screening should stop at age 81 or if the individual has not smoked in over 15 years.
Recently, experts from the National Lung Screening Trials (NLST) have encouraged a change to the recommendations for screening eligibility as the research has suggested many individuals at risk for lung cancer are not captured for screening by the current screening criteria. This group suggests that screening be expanded to include those with “heavy smoking histories who quit in the past 15 to 30 years (See this article for more information).”
Expansion of screening criteria could allow for increased early detection of lung cancers, resulting in improved long term outcomes and quality of life.
For more information on lung cancer screening visit:
In honor of lung cancer awareness month, I challenge those in high risk groups to talk with their primary care providers about lung cancer screening and, if you are still smoking, about assistance with quitting smoking. Various programs are available across the country to help you quit, and many are covered by insurance.
Other resources:
Smoking Cessation. Where do I start? – On OncoLink
Webucation: Lung Cancer Screening